INSULIN: Mechanism of Action & Metabolic Effects
understanding insulin's functions, mechanisms, and implications for health is fundamental in managing various metabolic disorders, including diabetes mellitus.
CLINICAL & APPLIED BIOCHEMISTRYDIABETES MELLITUS
9/7/20243 min read
🧬 INSULIN: Mechanism of Action & Metabolic Effects – A Lifeline in Glucose Balance
Imagine your body as a finely tuned orchestra, where every instrument must follow the conductor’s baton to maintain harmony. In the grand symphony of metabolism, insulin is that master conductor—subtle yet powerful, regulating energy use, storage, and balance.
But what makes insulin such a central figure in health and disease?
Let’s break it down into understandable insights, blending biochemistry with the latest research updates.
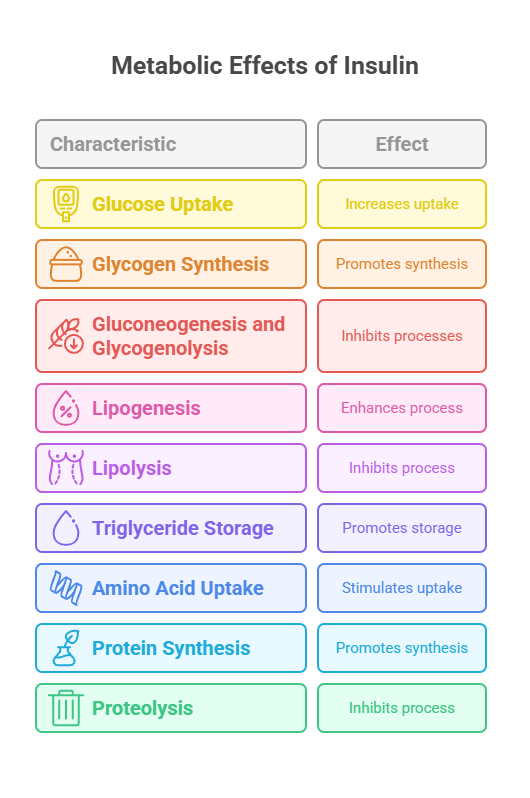
🔁 Metabolic Effects of Insulin: Master of Anabolism
Insulin doesn't just manage glucose—it commands multiple metabolic roads:
1. On Carbohydrate Metabolism
Increases glucose uptake (via GLUT-4)
Promotes glycogen synthesis in the liver and muscles
Inhibits gluconeogenesis and glycogenolysis
2. On Lipid Metabolism
Enhances lipogenesis (fat synthesis) in the liver and adipose tissue
Inhibits lipolysis by decreasing hormone-sensitive lipase activity
Promotes storage of triglycerides
3. On Protein Metabolism
Stimulates amino acid uptake
Promotes protein synthesis
Inhibits proteolysis (protein breakdown)
🧪 What Is Insulin?
Insulin is a peptide hormone produced by the beta cells of the pancreas (in the islets of Langerhans). It plays a vital role in glucose homeostasis, ensuring that blood sugar levels remain within a safe range.
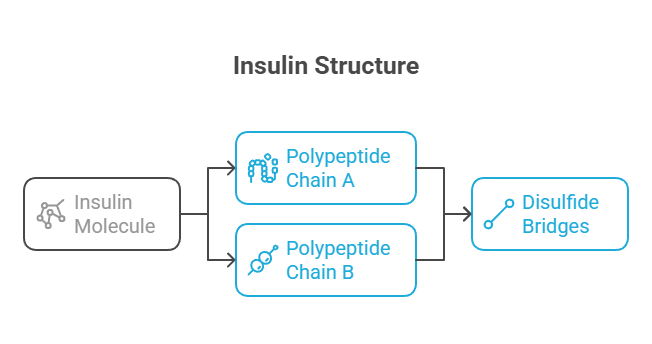
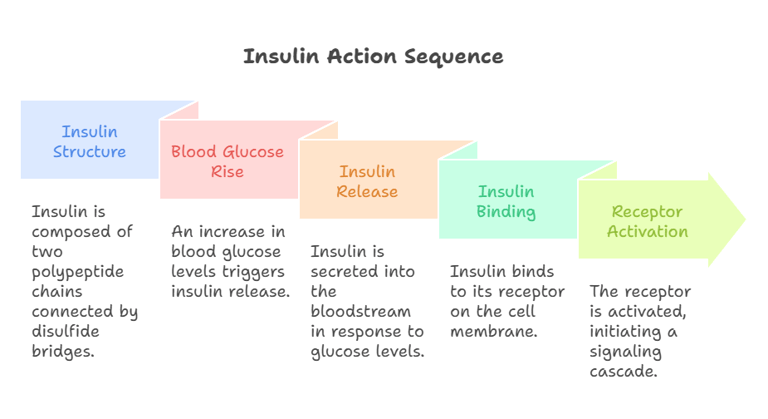
🔹 Structure: It's composed of two polypeptide chains (A and B) connected by disulfide bridges.
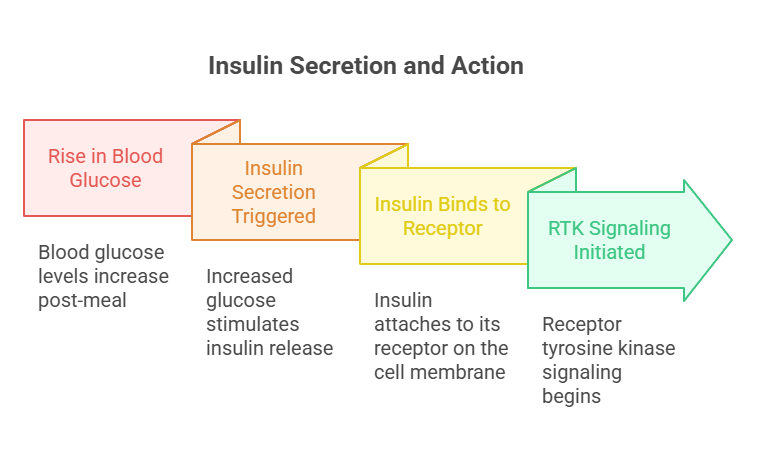
🔹 Secretion Trigger: A rise in blood glucose (especially post-meal) stimulates insulin release.
⚙️ Mechanism of Action: How Does Insulin Work?
Insulin binds to its receptor on the cell membrane—a classic example of receptor tyrosine kinase (RTK) signaling. Here’s a simplified flow:
🔄 Step-by-Step Process:
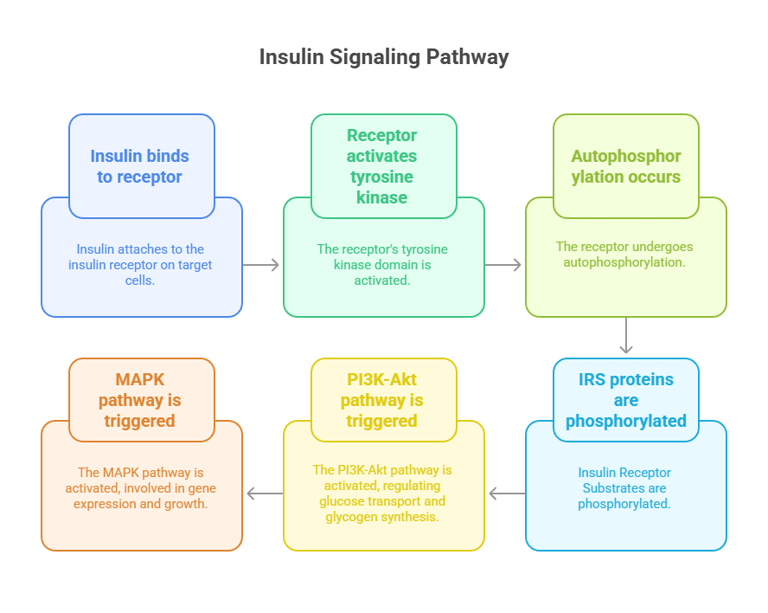
Insulin binds to the insulin receptor on target cells (muscle, fat, liver).
This activates the intrinsic tyrosine kinase domain, leading to autophosphorylation of the receptor.
The receptor phosphorylates Insulin Receptor Substrates (IRS) proteins.
This triggers two major pathways:
PI3K-Akt pathway → regulates glucose transport and glycogen synthesis.
MAPK pathway → is involved in gene expression and growth.
🧬 The PI3K-Akt pathway is (especially) important because it stimulates:
Translocation of GLUT-4 transporters to the plasma membrane in muscle and fat cells → promoting glucose uptake.
Glycogen synthesis via inhibition of glycogen synthase kinase-3 (GSK-3).
Protein synthesis and inhibition of apoptosis.
📌 Clinical Link: In Type 2 Diabetes, insulin may bind normally, but downstream signaling (especially PI3K-Akt) is impaired, leading to insulin resistance.
🧠 Fun Fact: Insulin also acts in the central nervous system, influencing appetite regulation and cognition—this is an area of growing interest in neuroendocrinology.
💡 In a Nutshell: The Takeaway
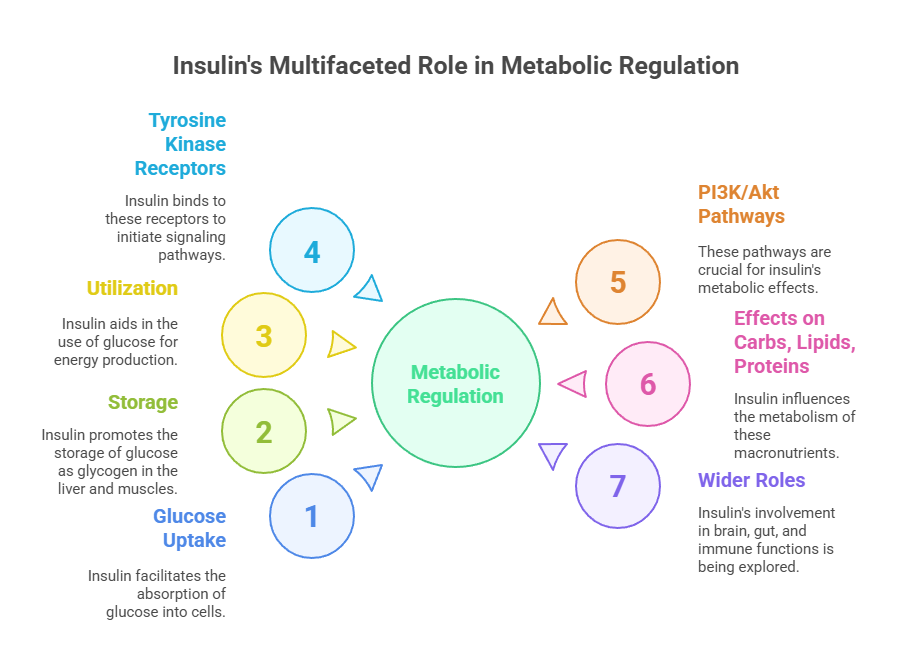
Insulin is an anabolic hormone that promotes glucose uptake, storage, and utilization.
It acts via tyrosine kinase receptors and intracellular signaling pathways (mainly PI3K/Akt).
Its effects span across carbs, lipids, and proteins.
Research is now revealing its wider roles in the brain, gut, and even immune responses.
Therapeutic innovations are targeting insulin signaling to combat diabetes and metabolic disorders more precisely.
🔬 Current Research Trends: What’s New in Insulin Science?
🌟 1. Dual Role of Insulin in the Brain
New studies show insulin resistance in the brain may contribute to Alzheimer’s disease ("Type 3 Diabetes").
Insulin signaling in the hypothalamus affects appetite, thermogenesis, and energy balance.
🌟 2. Precision Insulin Therapy
Research is underway to develop glucose-responsive "smart insulin", which adjusts its action based on real-time glucose levels—this could transform diabetes care.
🌟 3. Insulin and the Microbiome
Gut microbiota appears to influence insulin sensitivity—dysbiosis (imbalanced flora) may trigger insulin resistance.
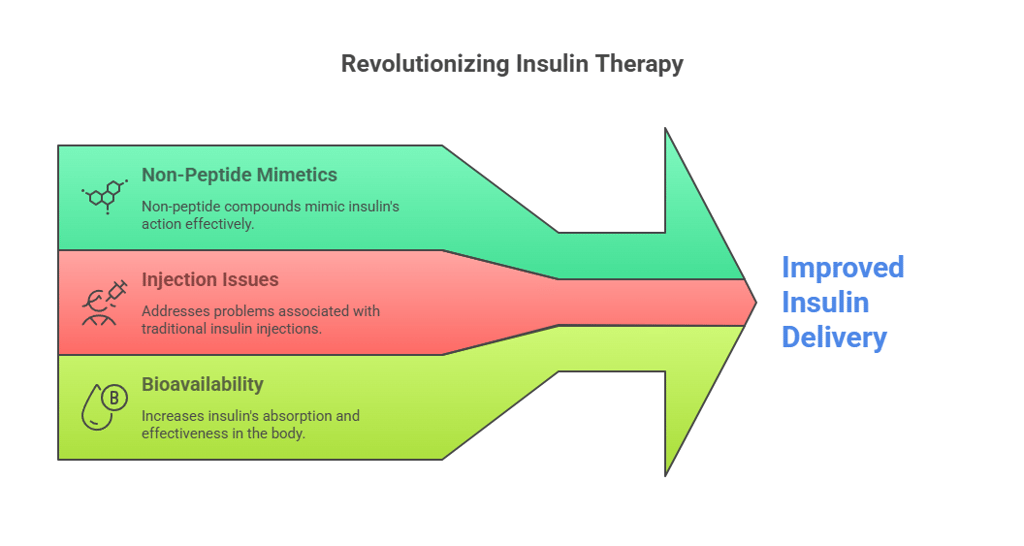
🌟 4. Insulin Mimetics
Scientists are exploring non-peptide insulin mimetics to bypass injection-related issues and improve bioavailability.
🩺 Clinical Relevance: Why Should We Care?
Whether you’re a medical student, clinician, or curious learner, insulin is more than a hormone—it’s a window into understanding metabolic health, obesity, cardiovascular risk, and diabetes. With over 500 million people globally living with diabetes, understanding insulin isn't just academic—it's essential.
BLOG
Join us to explore medical biochemistry intricacies.
WRITE TO US
© 2024. All rights reserved.
