Gastric Juice & Saliva Analysis
Gastric function tests assess the stomach's ability to secrete gastric juice, which is essential for digestion. These tests help diagnose conditions like gastric ulcers, Zollinger-Ellison syndrome, pernicious anemia, and gastritis.
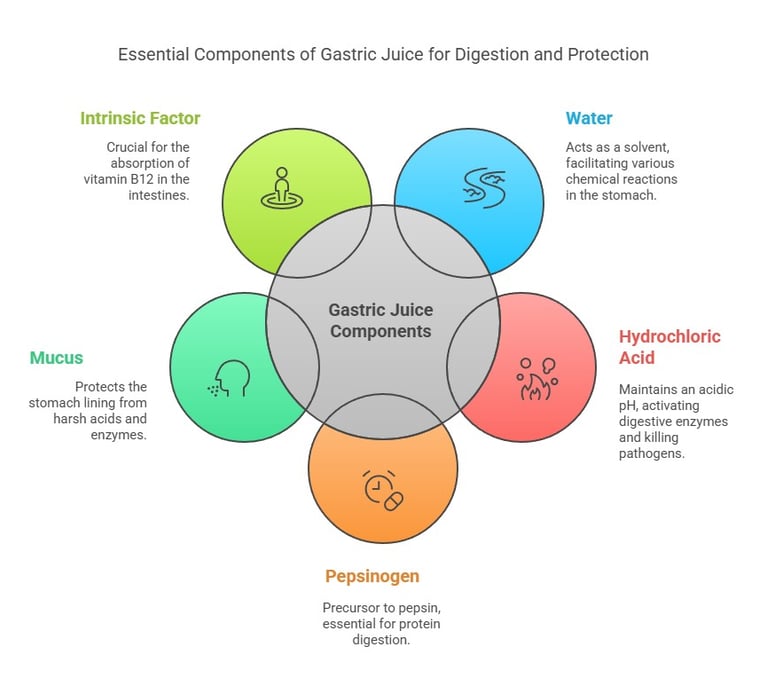
Key Components of Gastric Juice
Water: A Major component that acts as a solvent.
Hydrochloric Acid (HCl): Maintains acidic pH (~1-2), activates pepsinogen to pepsin, and kills pathogens.
Pepsinogen: Precursor of pepsin, which digests proteins.
Mucus: Protects the stomach lining from acid and enzymes.
Intrinsic Factor: Essential for vitamin B12 absorption.
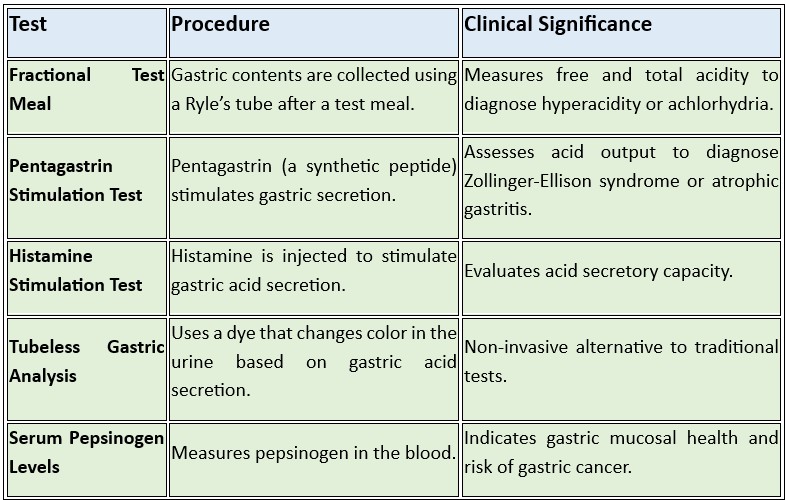
Types of Gastric Function Tests
Saliva: Formation, Regulation, Components, and Diagnostic Significance
Interpretation of Results
Hyperchlorhydria: Excessive acid secretion (e.g., Zollinger-Ellison syndrome).
Hypochlorhydria: Reduced acid secretion (e.g., chronic gastritis).
Achlorhydria: Absence of acid secretion (e.g., pernicious anemia).
Formation of Saliva
Produced by major salivary glands (parotid, submandibular, sublingual) and minor salivary glands.
Composed of 99% water and 1% organic and inorganic substances.
Secreted through acini (serous, mucous, or mixed) and transported via ducts.
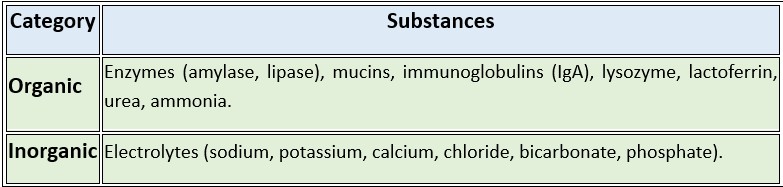
Components of Saliva
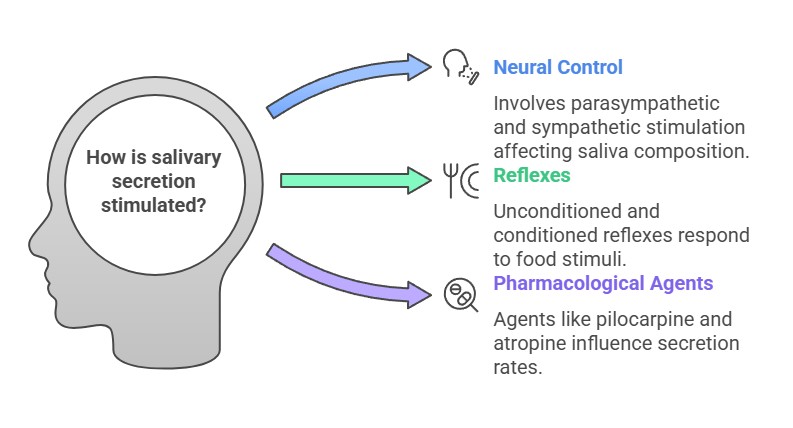
Factors Stimulating Salivary Secretion
Neural Control:
Parasympathetic Stimulation: Increases watery saliva (e.g., during eating).
Sympathetic Stimulation: Produces thick, mucous-rich saliva.
Reflexes:
Unconditioned Reflex: Triggered by food in the mouth.
Conditioned Reflex: Triggered by sight, smell, or thought of food.
Pharmacological Agents:
Pilocarpine stimulates secretion; atropine inhibits it.
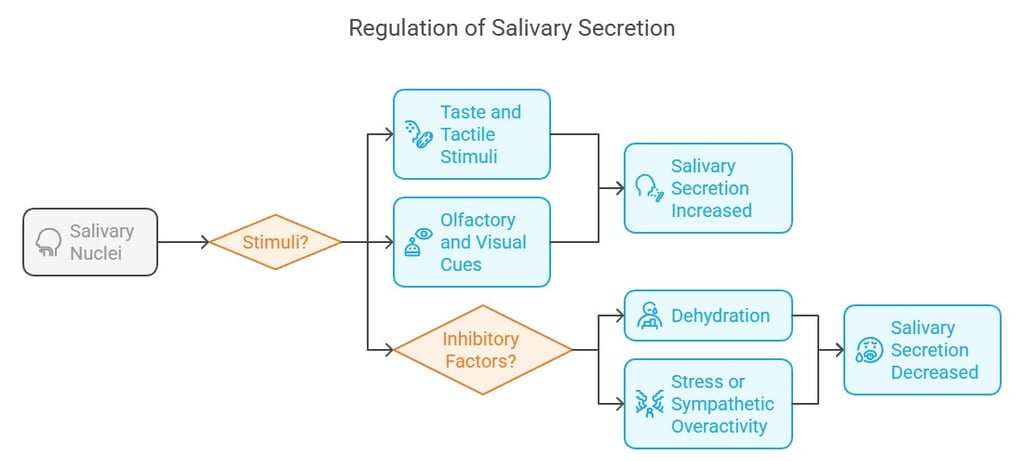
Regulation of Salivary Secretion
Controlled by the salivary nuclei in the brainstem.
Stimulated by:
Taste and tactile stimuli.
Olfactory and visual cues.
Inhibited by:
Dehydration.
Stress or sympathetic overactivity.
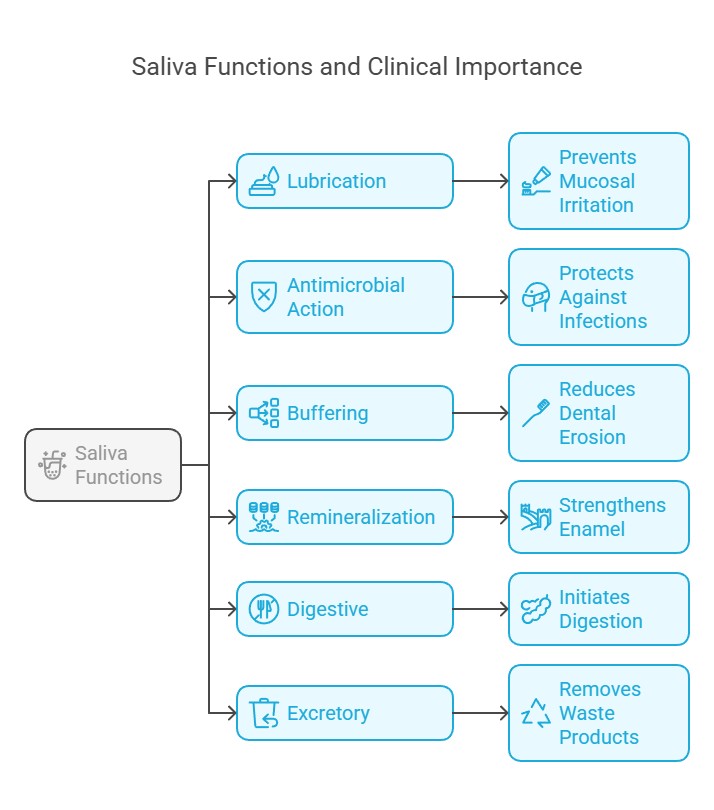
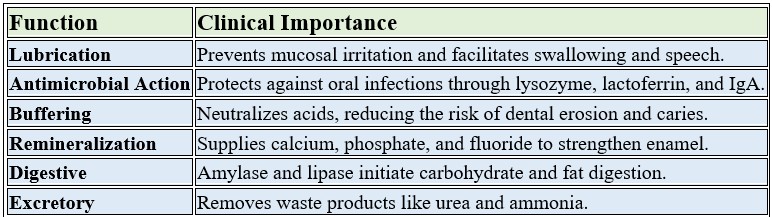
Functions of Saliva
Digestive:
Amylase: Breaks starch down into maltose.
Lipase: Initiates fat digestion.
Protective:
Lysozyme and IgA: Antimicrobial action.
Mucins: Lubricate and protect oral tissues.
Buffering:
Bicarbonate neutralizes acids, preventing dental caries.
Excretory:
Removes waste products like urea and ammonia.
Diagnostic:
Reflects systemic health (e.g., glucose levels in diabetes, cortisol in stress).
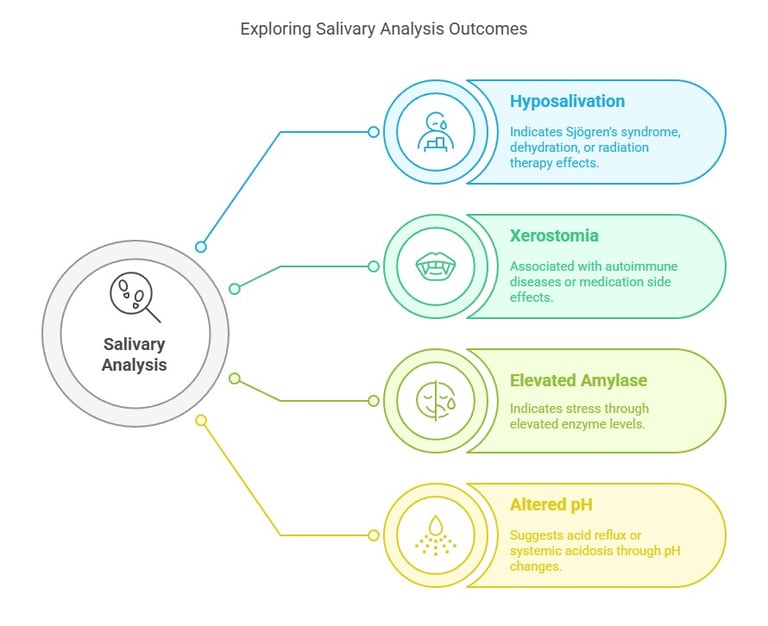
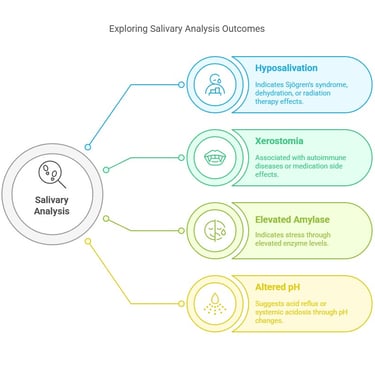
Diagnostic Significance
Hyposalivation: Indicates Sjögren’s syndrome, dehydration, or radiation therapy effects.
Xerostomia (Dry Mouth): Associated with autoimmune diseases or medication side effects.
Salivary Biomarkers:
Elevated amylase: Indicates stress.
Altered pH: Suggests acid reflux or systemic acidosis.
Clinical Aspects of Saliva and Salivary Glands
Saliva and salivary glands play crucial roles in maintaining oral and systemic health. Their dysfunction can lead to various clinical conditions, which are significant in both diagnostic and therapeutic contexts. Let’s explore these aspects in detail:
1. Clinical Conditions Related to Saliva and Salivary Glands
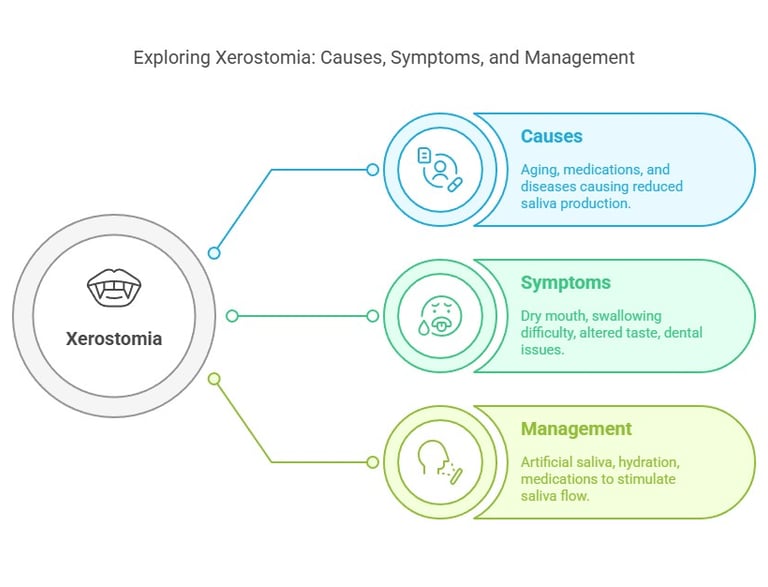
a) Xerostomia (Dry Mouth)
Cause:
Reduced salivary secretion due to aging, medications (e.g., antihistamines, diuretics), or systemic diseases (e.g., Sjögren’s syndrome, diabetes).
Symptoms:
Dryness in the mouth, difficulty swallowing, altered taste, and increased risk of dental caries.
Management:
Artificial saliva substitutes, hydration, and medications like pilocarpine to stimulate salivary flow.
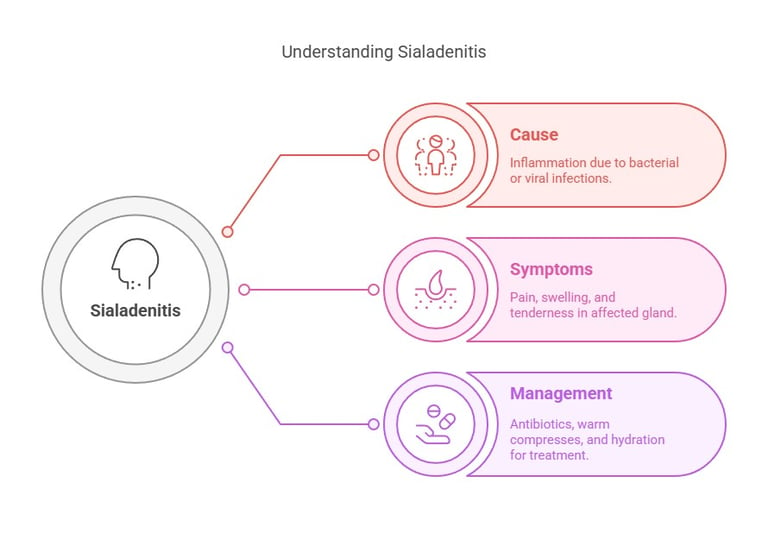
b) Sialadenitis
Cause:
Inflammation of salivary glands due to bacterial or viral infections (e.g., mumps, Staphylococcus aureus).
Symptoms:
Pain, swelling, and tenderness in the affected gland.
Management:
Antibiotics for bacterial infections, warm compresses, and hydration.
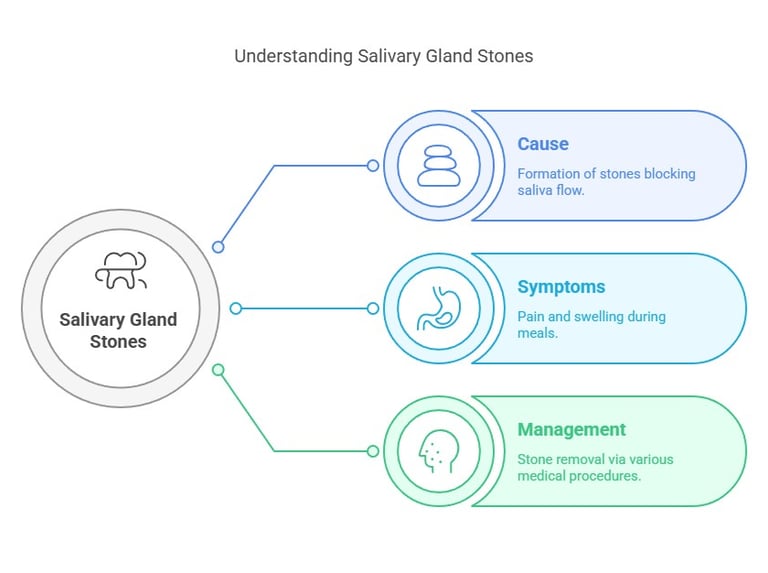
c) Salivary Gland Stones (Sialolithiasis)
Cause:
Formation of calcium-rich stones in salivary ducts, obstructing saliva flow.
Symptoms:
Pain and swelling during meals, as saliva secretion increases.
Management:
Removal of stones via sialography, lithotripsy, or surgical intervention.
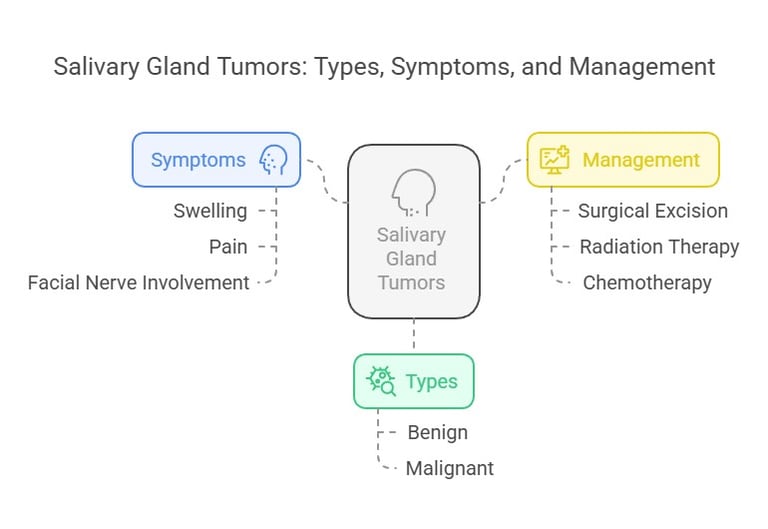
d) Tumors of Salivary Glands
Types:
Benign (e.g., pleomorphic adenoma) and malignant (e.g., mucoepidermoid carcinoma).
Symptoms:
Swelling, pain, and sometimes facial nerve involvement.
Management:
Surgical excision, radiation therapy, or chemotherapy.
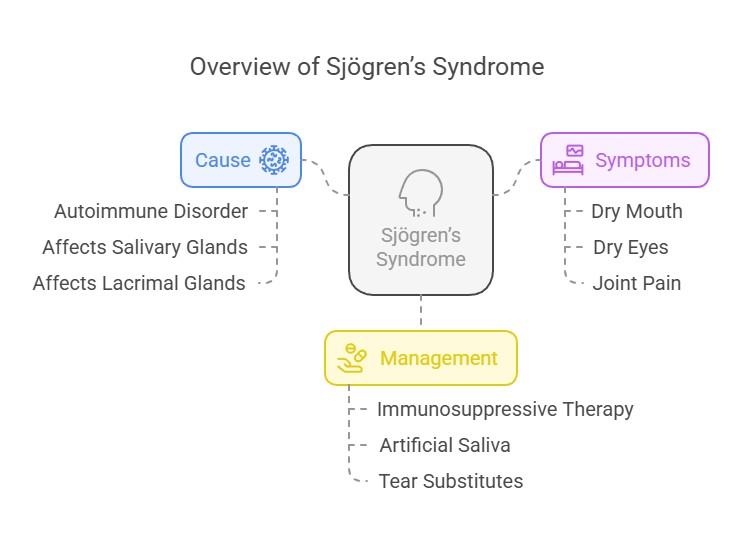
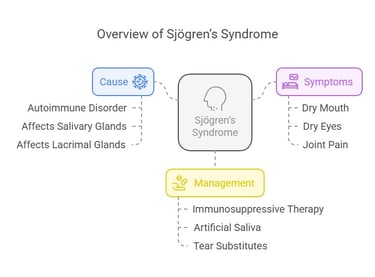
e) Sjögren’s Syndrome
Cause:
Autoimmune disorder affecting salivary and lacrimal glands.
Symptoms:
Dry mouth, dry eyes, and systemic manifestations like joint pain.
Management:
Immunosuppressive therapy, artificial saliva, and tear substitutes.
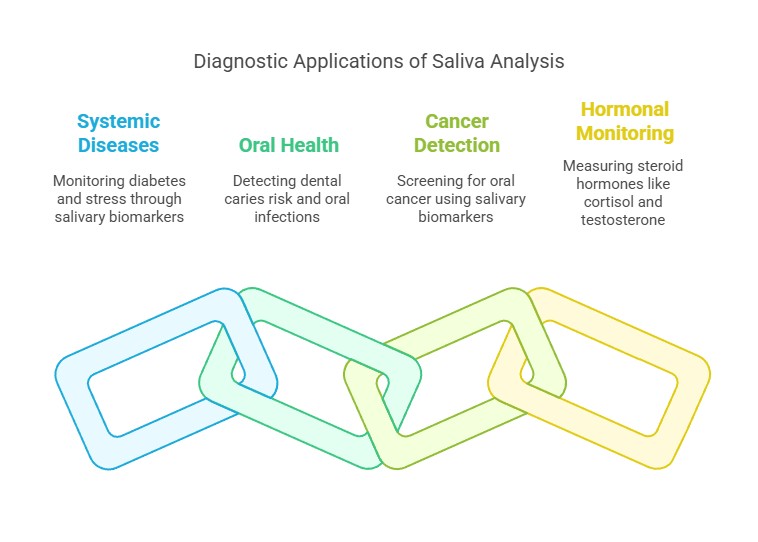
2. Diagnostic Significance of Saliva
Saliva serves as a non-invasive diagnostic tool for various conditions:
Systemic Diseases:
Salivary biomarkers (e.g., glucose, cortisol) help monitor diabetes and stress.
Oral Health:
Saliva analysis detects dental caries risk, periodontal disease, and oral infections.
Cancer Detection:
Salivary biomarkers like p53 and HER2 are used in oral cancer screening.
Hormonal Monitoring:
Saliva is used to measure steroid hormones like cortisol and testosterone.
3. Functions of Saliva in Clinical Context
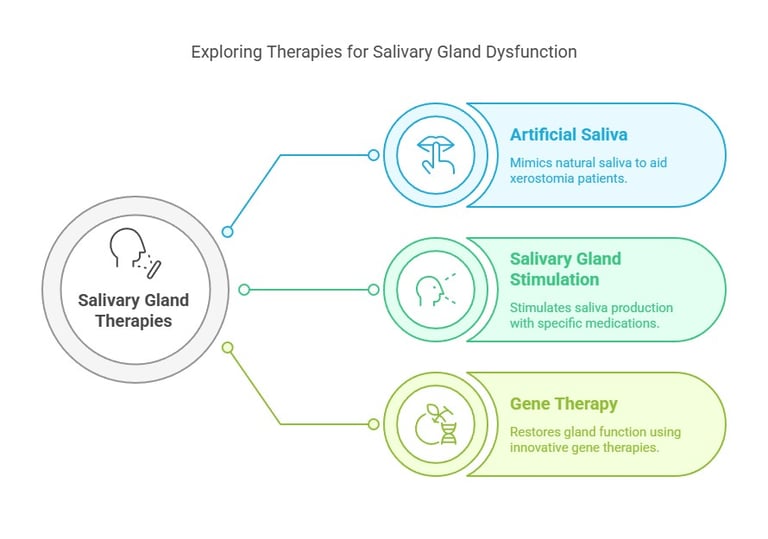
4. Therapeutic Applications
Saliva and salivary glands are targeted in various therapies:
Artificial Saliva:
Used in xerostomia to mimic natural saliva’s protective functions.
Salivary Gland Stimulation:
Medications like pilocarpine and cevimeline stimulate salivary secretion.
Gene Therapy:
Emerging treatments aim to restore salivary gland function in conditions like Sjögren’s syndrome.
Conclusion
Saliva and salivary glands are integral to oral and systemic health, and their dysfunction can lead to significant clinical challenges. Advances in saliva-based diagnostics and therapies continue to enhance patient care.
BLOG
Join us to explore medical biochemistry intricacies.
WRITE TO US
© 2024. All rights reserved.
