Diabetes Mellitus: An In-Depth Guide
Diabetes mellitus (DM) is a chronic metabolic disorder characterized by persistent hyperglycemia resulting from defects in insulin secretion, insulin action, or both.
It is a significant global health problem, affecting millions of individuals worldwide, with profound clinical, social, and economic implications. This article provides detailed insights into the types, clinical significance, associated disorders, symptoms, hormonal effects, blood glucose regulation, and lab diagnostic tests of diabetes mellitus.
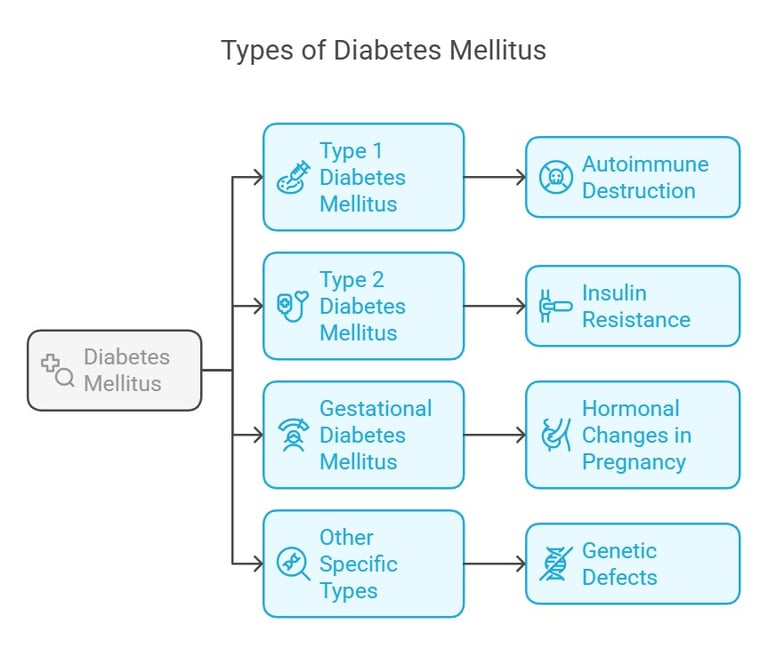
Types of Diabetes Mellitus and Clinical Significance
Diabetes mellitus is broadly classified into four main types:
Type 1 Diabetes Mellitus (T1DM):
Cause: Autoimmune destruction of pancreatic β-cells leading to absolute insulin deficiency.
Clinical Significance: Commonly manifests in childhood or adolescence. Patients require lifelong insulin therapy. Without treatment, ketoacidosis can occur, which may be life-threatening.
Type 2 Diabetes Mellitus (T2DM):
Cause: Combination of insulin resistance and relative insulin deficiency.
Clinical Significance: Primarily affects adults, though increasing cases in children are linked to rising obesity rates. It can lead to complications like cardiovascular diseases, neuropathy, nephropathy, and retinopathy.
Gestational Diabetes Mellitus (GDM):
Cause: Glucose intolerance was first detected during pregnancy due to hormonal changes affecting insulin action.
Clinical Significance: Increases the risk of adverse maternal and fetal outcomes and predisposes both the mother and child to T2DM later in life.
Other Specific Types: These include diabetes due to genetic defects of β-cell function, diseases of the exocrine pancreas (e.g., cystic fibrosis), drug-induced diabetes (e.g., corticosteroids), or endocrinopathies like Cushing's syndrome.
Disorders and Symptoms of Diabetes Mellitus
Diabetes mellitus is associated with a wide range of disorders, which can be classified as acute or chronic.
Acute Disorders:
Diabetic ketoacidosis (DKA) in T1DM.
Hyperosmolar hyperglycemic state (HHS) in T2DM.
Chronic Complications:
Microvascular: Diabetic retinopathy, nephropathy, and neuropathy.
Macrovascular: Coronary artery disease (CAD), peripheral arterial disease (PAD), and stroke.
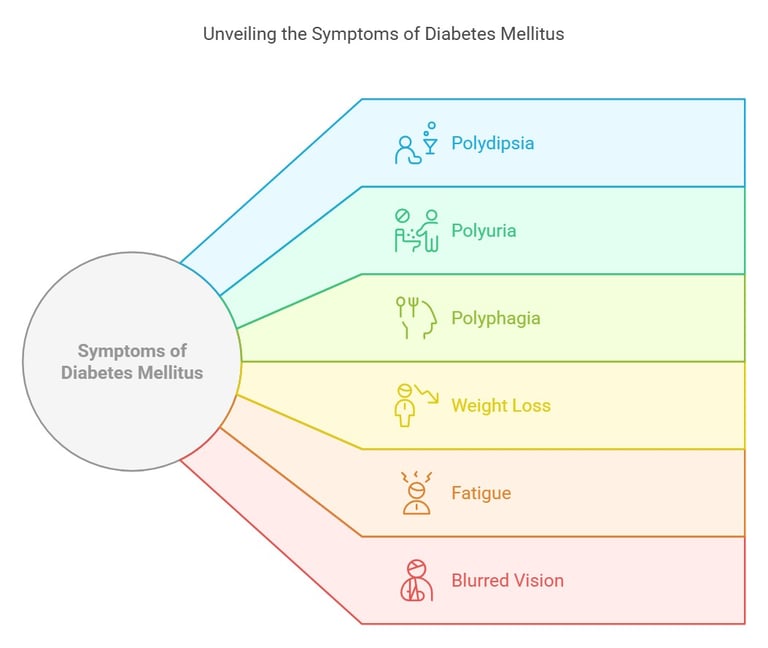
Common Symptoms:
Polydipsia (excessive thirst).
Polyuria (frequent urination).
Polyphagia (increased appetite).
Weight loss, fatigue, and blurred vision.
Slow-healing wounds or recurrent infections.
Disorders and Symptoms of Diabetes Mellitus
Role of Hormones and Blood Glucose Regulation
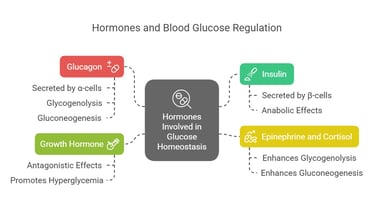
Hormones Involved in Glucose Homeostasis:
Insulin (anabolic hormone): Secreted by β-cells of the pancreas; promotes glucose uptake by cells and storage as glycogen.
Glucagon: Secreted by α-cells of the pancreas; stimulates glycogenolysis and gluconeogenesis to increase blood glucose levels.
Epinephrine and Cortisol: Stress hormones that enhance gluconeogenesis and glycogenolysis.
Growth Hormone: Antagonizes insulin's action, promoting hyperglycemia.
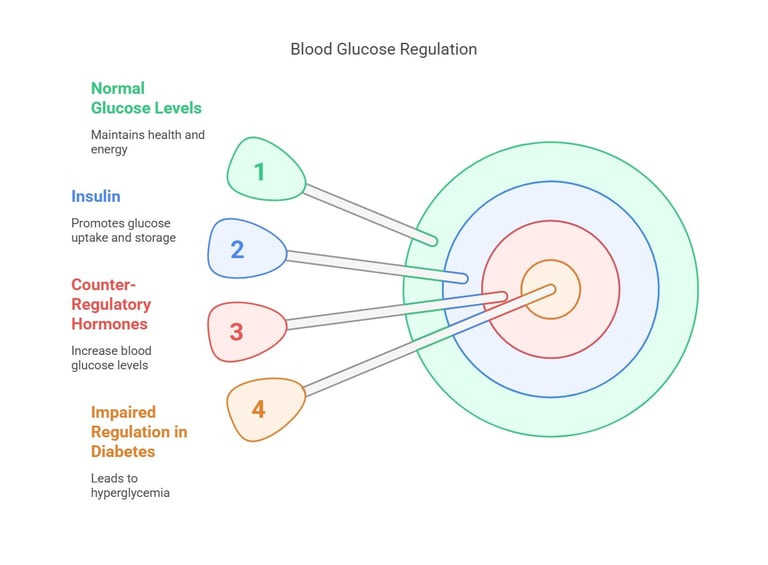
Blood Glucose Regulation: Under normal physiological conditions, a balance between insulin and counter-regulatory hormones maintains blood glucose levels between 70–110 mg/dL (fasting). In diabetes, this regulation is impaired, resulting in hyperglycemia.

Lab Diagnostic Tests of Diabetes Mellitus.
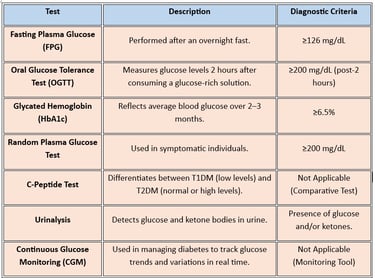
1. Fasting Plasma Glucose (FPG):
Performed after an overnight fast.
Diagnostic Criteria: ≥126 mg/dL.
2. Oral Glucose Tolerance Test (OGTT):
Measures glucose levels 2 hours after consuming a glucose-rich solution.
Diagnostic Criteria: ≥200 mg/dL (post-2 hours).
3. Glycated Hemoglobin (HbA1c):
Reflects average blood glucose over 2–3 months.
Diagnostic Criteria: ≥6.5%.
4. Random Plasma Glucose Test:
Used in symptomatic individuals.
Diagnostic Criteria: ≥200 mg/dL.
5. C-Peptide Test:
Differentiates between T1DM (low levels) and T2DM (normal or high levels).
6. Urinalysis:
Detects glucose and ketone bodies in urine.
7. Continuous Glucose Monitoring (CGM):
Used in managing diabetes to track glucose trends and variations in real-time.
Conclusion
Diabetes mellitus is a multifaceted condition with significant clinical implications. Understanding its types, underlying pathophysiology, clinical features, and diagnostic approaches is crucial for medical students and healthcare professionals.
Effective management requires early diagnosis, patient education, lifestyle modifications, and pharmacological interventions.

The 2025 Standards of Care in Diabetes
The 2025 Standards of Care in Diabetes, released by the American Diabetes Association (ADA), provide updated recommendations for diabetes management. Here are some key highlights:
Continuous Glucose Monitoring (CGM):
Recommended for individuals with Type 2 Diabetes (T2DM), even if they are not on insulin therapy. This helps in tracking blood glucose trends effectively.
Pharmacological Updates:
Expanded use of GLP-1 receptor agonists, not only for weight loss but also for cardiovascular and kidney health benefits.
Guidance on managing medication shortages and ensuring continuity of care.
Screening and Prevention:
Early screening for Type 1 Diabetes in individuals with a family history or genetic risk.
Emphasis on preventing Type 2 Diabetes through weight management and lifestyle interventions.
Nutrition and Lifestyle:
Encouragement of evidence-based eating patterns, including those rich in plant-based proteins and fiber, to achieve metabolic goals.
Expanded guidance on physical activity and behavioral health to improve outcomes.
Individualized Care:
Focus on tailoring treatment plans to individual needs, considering factors like age, comorbidities, and personal preferences.
Special Populations:
Updated recommendations for managing diabetes in older adults, pregnant women, and those with metabolic dysfunction-associated steatotic liver disease (MASLD).
Technology Integration:
Increased emphasis on using diabetes technology, such as insulin pumps and CGMs, to enhance patient care.
These guidelines aim to provide a comprehensive approach to diabetes care, focusing on improving health outcomes and quality of life for individuals with diabetes.
References: www.diabetesjournals.org www.professional.diabetes.org www.diabetes.org
BLOG
Join us to explore medical biochemistry intricacies.
WRITE TO US
© 2024. All rights reserved.
