Biochemistry of Bone & Teeth
🦷 Biochemistry of Teeth: Molecular Foundations of Dental Health. Bone and teeth are more than support structures—they are metabolically active, living tissues that reflect systemic health.”
Understanding the biochemical and structural composition of bones and teeth is essential for both medical and dental students. These tissues not only serve mechanical and protective functions but are also sites of mineral storage, remodeling, and important indicators of metabolic diseases.
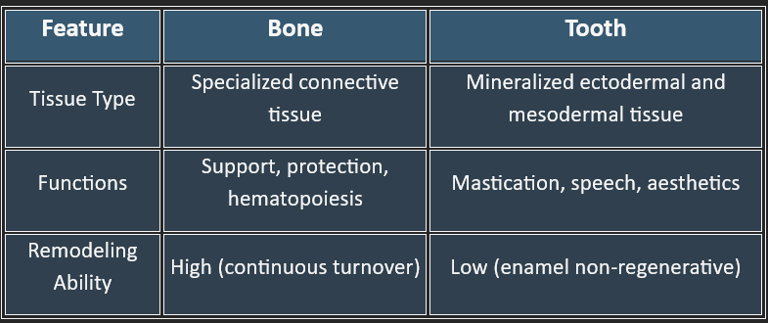
I. Overview of Bone and Tooth Tissue
II. Composition of Bone 🦴
The composition of the bone may be discussed by dividing it into three main parts:
A. Inorganic Components (~65%)
B. Organic Matrix (~35%)
C. Cellular Elements
A. Inorganic Components (~65%)
Predominantly hydroxyapatite crystals: Ca₁₀(PO₄)₆(OH)₂
Provides rigidity and compressive strength
Major minerals:
Calcium (Ca²⁺)
Phosphate (PO₄³⁻)
Trace elements: magnesium, sodium, fluoride
C. Cellular Elements
Osteoblasts: Bone-forming cells
Osteocytes: Mature cells embedded in matrix
Osteoclasts: Multinucleated cells that resorb bone
B. Organic Matrix (~35%)
Composed mainly of Type I collagen (~90%)
Gives tensile strength
Non-collagenous proteins:
Osteocalcin: Regulates calcium binding
Osteonectin: Binds mineral to collagen
Bone sialoprotein: Promotes mineralization
Proteoglycans: Hydration and structural organization
Teeth have four distinct tissue layers:
1. Enamel (Outer Layer)
2. Dentin
3. Cementum
4. Pulp
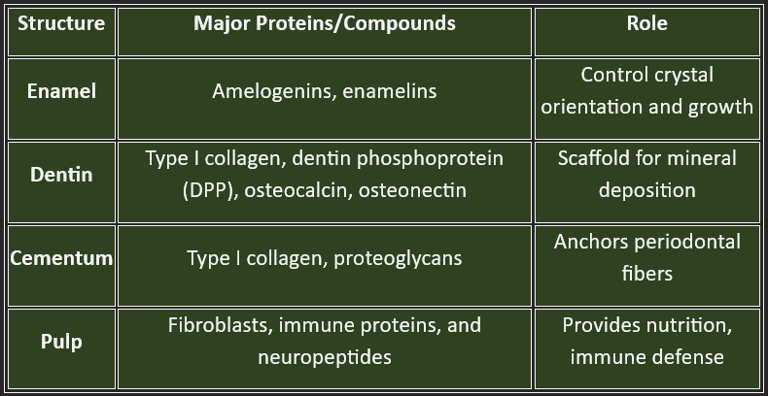
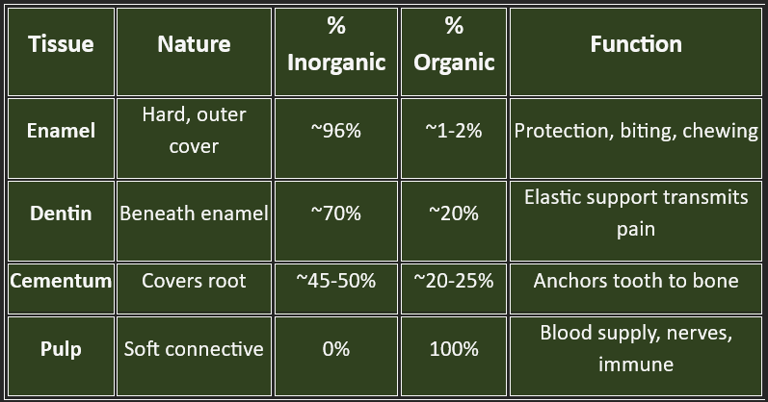
Biochemical Composition:
1. Inorganic Components (Mineral Phase) 2. Organic Components (Protein Matrix)
🦷 III. Composition of Teeth
1. Inorganic Components (Mineral Phase)
Hydroxyapatite Crystals: Ca10(PO4)6(OH)2
A key component of enamel, dentin, and cementum
Provides rigidity and strength
Can be replaced by fluorapatite Ca10(PO4)6F2Ca₁₀(PO₄) ₆F₂ for caries resistance
[Fluoride enhances resistance to demineralization by forming fluorapatite, a more acid-resistant mineral.]
IV. Developmental Biochemistry (Odontogenesis)
Tooth development involves sequential molecular signaling between epithelial and mesenchymal cells.
Key Stages:
Initiation – gene expression triggers the dental lamina.
Bud stage – cell proliferation (FGFs, BMPs active)
Cap stage – enamel organ forms, signaling pathways coordinate structure
Bell stage – differentiation into:
Ameloblasts (form enamel)
Odontoblasts (form dentin)
Key Molecules:
BMPs (Bone morphogenetic proteins)
FGFs (Fibroblast growth factors)
SHH (Sonic Hedgehog)
Wnt signaling
Disruption in these signals → tooth agenesis, enamel hypoplasia, or dentinogenesis imperfecta
🦷
1. Mineralization
Controlled deposition of hydroxyapatite on organic matrix
Enzymes like alkaline phosphatase and matrix metalloproteinases (MMPs) are vital
Vitamin D, calcium, and phosphate are essential cofactors
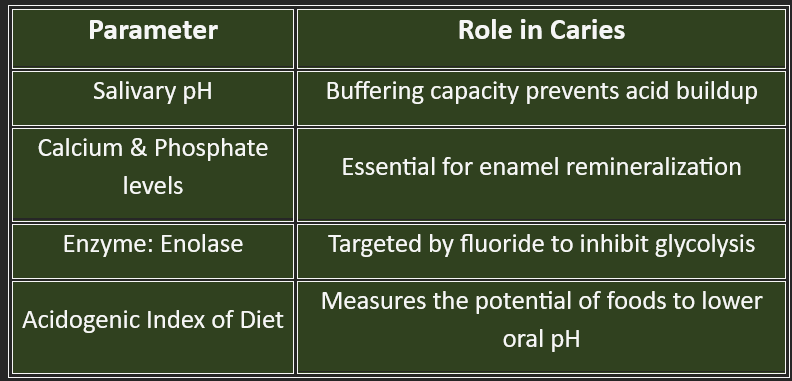
2. Demineralization and Remineralization
Demineralization: Loss of calcium/phosphate from enamel in acidic pH (<5.5)
Remineralization: Recovery of minerals from saliva, fluoride, and diet
Saliva acts as a natural buffer with calcium, phosphate, and bicarbonate
V. Biochemical Processes in Tooth Health
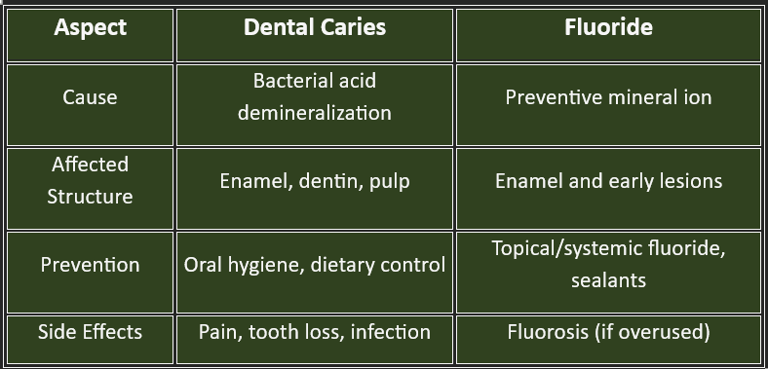
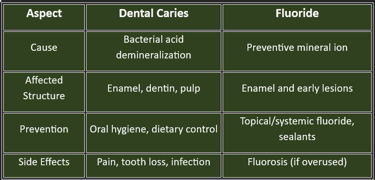
VI. Biochemistry of Dental Caries 🦠
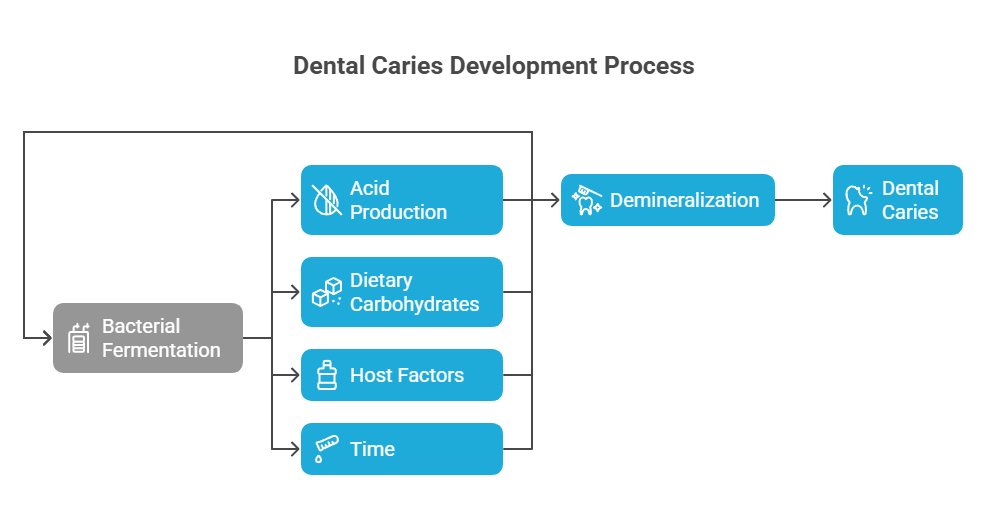
Dental Caries (Process):-
Caused by acid-producing bacteria (e.g., Streptococcus mutans) in plaque
Bacteria ferment dietary sugars → produce lactic acid
Acid dissolves enamel (Demineralization)
Cariogenic Pathway:
Glucose → Pyruvate → Lactic Acid → Enamel Demineralization
Protective factors:
Salivary proteins (mucins, lysozyme, lactoferrin)
Fluoride use
Xylitol (non-fermentable sweetener)
“Tooth decay is not just a hole in the enamel—it’s a dynamic biochemical war between demineralization and remineralization.”
Dental caries (commonly known as tooth decay) is one of the most prevalent non-communicable diseases globally.
I. 🦷What are Dental Caries?
Dental caries is a multifactorial infectious disease characterized by the progressive demineralization of tooth enamel and dentin caused by acids produced by bacterial fermentation of dietary carbohydrates.
Etiology:
Primary causative agent: Streptococcus mutans, Lactobacilli, Actinomyces
Diet: High in fermentable sugars (especially sucrose)
Host factors: Tooth morphology, saliva flow, fluoride exposure
Time: Repeated and prolonged exposure to acidogenic conditions
🔬 II. Pathophysiology: From Sugar to Cavity
1. Bacterial Metabolism
Oral bacteria ferment carbohydrates → produce lactic acid
pH drops below 5.5 (critical pH) → enamel demineralization begins
2. Demineralization
Acid dissolves the hydroxyapatite crystals of enamel
Ca²⁺ and PO₄³⁻ ions are lost → formation of a porous subsurface lesion
3. Progression to Dentin
Once the enamel barrier is breached, acids and bacteria infiltrate dentin
Dentin is softer, less mineralized, and more prone to destruction
Pain and sensitivity may arise when approaching the pulps
III. The Role of Fluoride
Fluoride (F⁻) is a naturally occurring ion that significantly strengthens enamel and inhibits caries formation.
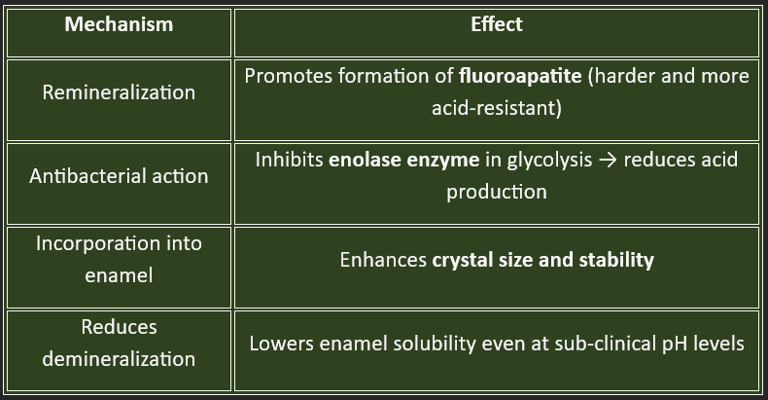
Mechanisms of Action:
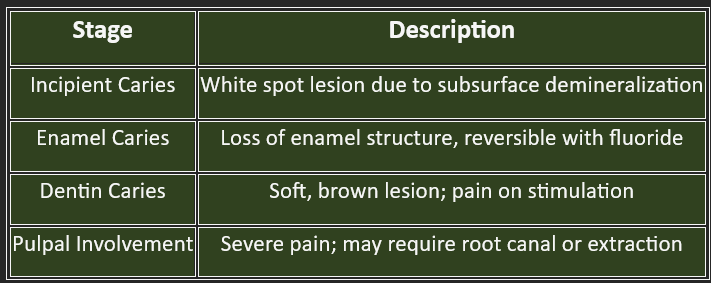
VII. Clinical Aspects of Dental Caries
A. Stages of Caries
🩺 Clinical Relevance for Medical/Dental Students
Understanding caries prevention and enamel remineralization helps in public health campaigns.
Fluoride therapy, dietary counseling, and saliva analysis are rooted in biochemical knowledge.
Tooth development defects may signal underlying genetic syndromes.
Metabolic bone diseases (e.g., rickets, osteogenesis imperfecta) often present with oral signs.
C. Treatment Strategies
Remineralization with topical fluoride or CPP-ACP (casein phosphopeptide-amorphous calcium phosphate)
Restorations: composite resins, glass ionomer cement, amalgam
Endodontic treatment: in advanced cases
B. Diagnosis
Clinical inspection (mirror and explorer)
Radiographs (bitewing, periapical)
Laser fluorescence (e.g., DIAGNOdent)
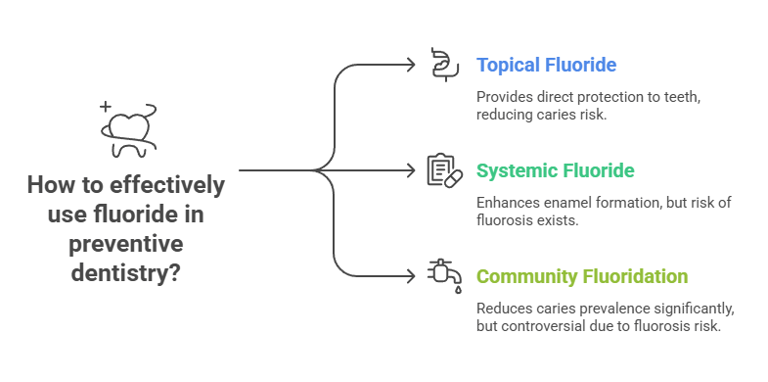
VIII. Fluoride in Preventive Dentistry
Sources of Fluoride:
Topical: Toothpaste, mouth rinses, varnishes
Systemic: Fluoridated water (optimal level ~0.7 ppm), supplements
Community Fluoridation:
Reduces dental caries prevalence by up to 60%
Controversy over fluorosis risk (mottled enamel with excessive intake)
Dental Fluorosis:
Caused by chronic overexposure to fluoride during enamel formation
Severity: Ranges from mild white spots to severe brown stains and pitting
IX. Biochemical Insights🔍
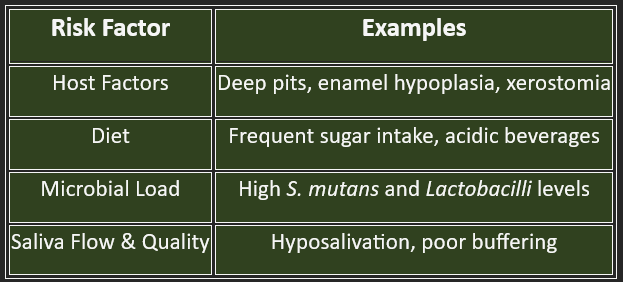
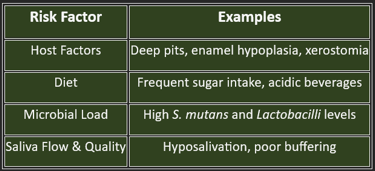
X. Caries Risk Assessment
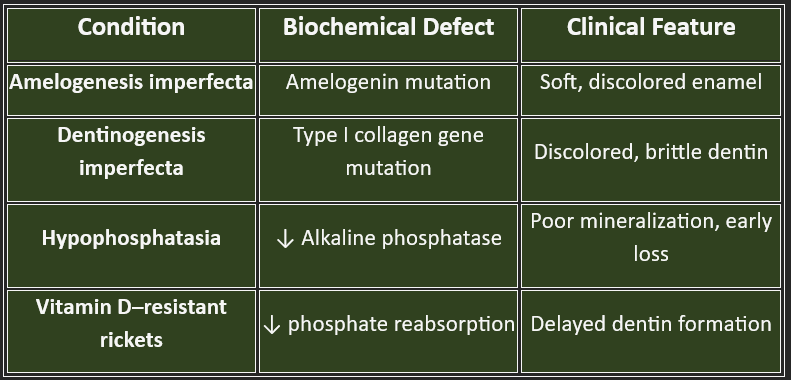
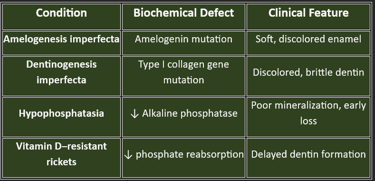
XI. Genetic Disorders Affecting Teeth🧬
Summary Table 💡 Final Thoughts
💡 Final Thoughts
Dental caries reflects the complex interplay between bacterial metabolism, host resistance, and environmental factors.
Fluoride acts as a powerful, scientifically proven protector, shifting the balance toward remineralization and oral resilience.
For medical students, particularly in dentistry and pediatrics, understanding this process is essential for effective public health planning, patient counseling, and clinical interventions.
“To preserve a tooth is to preserve a patient's smile, nutrition, and self-esteem.”
BLOG
Join us to explore medical biochemistry intricacies.
WRITE TO US
© 2024. All rights reserved.
